Why is this medication prescribed?
Emergency medical care is combined with the use of naloxone injections and naloxone prefilled auto-injection devices (Evzio) to reverse the potentially fatal consequences of an opiate (narcotic) overdose. To counteract the effects of the opiates administered during surgery, naloxone injection is also utilised following surgery. To lessen the effects of opiates taken by the expectant mother prior to delivery, naloxone injection is administered to infants. The drug naloxone injection belongs to the group of drugs known as opiate antagonists. To treat harmful symptoms brought on by excessive levels of opiates in the blood, it functions by inhibiting the effects of opiates.
How should this medicine be used?
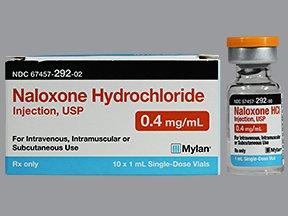
Naloxone injection is available as a liquid solution that can be administered intravenously, intramuscularly, or subcutaneously (just under the skin). Additionally, it is available as a prefilled auto-injection device with a solution that can be administered subcutaneously or intramuscularly. To treat opiate overdoses, it is often administered as needed.
If you overdose on opiates, you probably won’t be able to heal yourself. Make certain that your family, carers, and those who spend time with you are aware of the signs of an overdose, how to administer naloxone injections, and what to do until emergency medical assistance arrives. You and your family members will be shown how to use the medication by your doctor or pharmacist. You should read the directions that come with the nasal injection, as well as anyone else who might have to administer the medication. For the directions, speak to your pharmacist or go to the manufacturer’s website.
Buprenorphine (Belbuca, Buprenex, Butrans), pentazocine (Talwin), and other opiates may not be completely reversed by naloxone injection, necessitating multiple naloxone doses.
If you overdose on opiates, you probably won’t be able to heal yourself. You should make sure that your family, carers, or those who spend time with you are aware of the signs of an overdose, how to administer naloxone, and what to do while waiting for emergency assistance. You and your family members will be shown how to administer the medication by your doctor or pharmacist. You should study the device’s instructions and practise using the training tool that comes with the drug, as well as anyone else who might need to give it. For instructions, speak to your pharmacist or go to the manufacturer’s website. Even someone who has not received training to administer naloxone should attempt to do so in an emergency.
If an automatic injection device has been given to you, you should maintain it close by at all times in case an opioid overdose occurs. Make sure you replace your device when it reaches its expiration date by keeping track of it. Check the device’s solution from time to time. Make an appointment with your doctor to obtain a new injection device if the fluid is cloudy or contains particles.
An electronic voice system with step-by-step instructions is built into the automatic injection device. These instructions can be followed by the person giving you the naloxone injection, but he or she should be aware that there is no need to wait for the speech system to complete one step before moving on to the next. The voice system may occasionally malfunction, making it impossible for someone to hear directions. Even if the voice system is malfunctioning, the gadget will nonetheless continue to function and continue to inject the medication.
Excessive sleepiness, resistance to being awakened by loud voices or by strong pressure on the centre of the chest, shallow or halted breathing, and small pupils are all signs of an opioid overdose (black circles in the centre of the eyes). Someone should administer your first dosage of naloxone into the muscle or just beneath the skin of your thigh if they see that you are exhibiting these symptoms. In an emergency, the drug may be injected via your clothing. The person who gave you the naloxone injection should immediately dial 911, stay by your side, and keep a close eye on you until aid arrives. After receiving a naloxone injection, your symptoms can come back in a short while. If your symptoms come back, the person should provide another dose of naloxone using a fresh automated injection device. If symptoms return before medical assistance comes, more injections may be administered every 2-3 minutes.
Only one use should be made of each prefilled automatic injection device before it is discarded. Even if you did not inject the medication, do not attempt to reinsert the red safety shield after removing it from the auto-injection device. Instead of throwing away the discarded gadget, replace it in the outer casing. Find out from your physician or pharmacist how to properly discard used injectable equipment.
Other uses for this medicine
Ask your doctor or pharmacist for more details if you believe this drug should be used for something else.
What special precautions should I follow?
Before using naloxone injection,
- If you have an allergy to naloxone injection, any other drugs, or any of the chemicals in naloxone injection, let your doctor and pharmacist know right once. For a list of the ingredients, consult your pharmacist or the manufacturer’s patient information.
- Inform your doctor and pharmacist about any additional prescription and over-the-counter drugs, vitamins, dietary supplements, and herbal products you are now taking or intend to use. The likelihood that you will experience severe side effects from naloxone injection may be increased by a number of drugs that influence your heart or blood pressure. Make sure to disclose to your doctor every drug you are taking.
- If you have or have had had heart, renal, or liver disease, let your doctor know.
- If you are breastfeeding a child or intend to become pregnant, let your doctor know. If you receive a naloxone injection while pregnant, your doctor may need to keep a close eye on your developing baby after the injection.
What side effects can this medication cause?
Side effects from naloxone injection are possible. If any of these symptoms are severe or do not go away, let your doctor know right once:
- Redness, stinging, or discomfort at the injection site
- Sweating
- Hot flashes or flushing
Some adverse effects can be very harmful. You should seek immediate medical attention if you encounter any of these symptoms:
- Irregular, hammering, or quick heartbeat
- Hearing voices or perceiving nonexistent objects (hallucinations)
- Consciousness loss
- Seizures
- Body aches, diarrhoea, a rapid heartbeat, a fever, runny nose, sneezing, sweating, yawning, nausea, vomiting, anxiety, restlessness, irritability, shaking or trembling, weakness, and the appearance of hair standing on end on the skin are symptoms of opiate withdrawal.
- More tears than usual (in babies treated with naloxone injection)
- Greater than average reflexes (in babies treated with naloxone injection)
Other negative effects after naloxone injection are possible. If you have any strange side effects while taking this medicine, let your doctor know.
You or your doctor can submit a report to the Food and Drug Administration’s (FDA) MedWatch Adverse Event Reporting programme online or by phone if you have a serious side event (1-800-332-1088).
What should I know about storage and disposal of this medication?
Keep this medication tightly closed in the original container and out of the reach of children. Keep the automatic injection device dark and at normal temperature. Dispose of the automatic injection device in a safe manner if the red safety guard has been removed.
Unused prescriptions must be disposed of carefully to prevent pets, kids, and other people from ingesting them. You should not, however, dispose of this medication in the toilet. Instead, utilising a medicine take-back programme is the easiest approach to get rid of your medication. To find out about take-back programmes in your area, speak with your pharmacist or the garbage/recycling department in your city. If you do not have access to a take-back programme, see the FDA’s Safe Disposal of Medicines website at http://goo.gl/c4Rm4p for additional information.
As many containers (such as weekly pill minders and those for eye drops, creams, patches, and inhalers) are not child-resistant and are simple for young children to open, it is crucial to keep all medications out of sight and out of reach of children. Always lock safety caps and promptly stash medication up and away from young children where it is out of their sight and reach to prevent poisoning. http://www.upandaway.org
What other information should I know?
Do not share your medication with anybody else. Any queries you may have regarding medication refills should be directed to your pharmacist.
You should keep a written record of every medication you take, including any over-the-counter (OTC) items, prescription drugs, and dietary supplements like vitamins and minerals. This list should be brought with you whenever you see a doctor or are admitted to the hospital. You should always have this information with you in case of emergencies.
Brand names
- Narcan®
- Evzio®