Why is this medication prescribed?
Levonorgestrel intrauterine system (Liletta, Kyleena, Mirena, Skyla) is used to prevent pregnancy. The Mirena brand intrauterine system is also used to treat heavy menstrual bleeding in women who want to use an intrauterine system to prevent pregnancy. Levonorgestrel is in a class of medications called hormonal contraceptives. Levonorgestrel intrauterine system works by thinning the lining of the uterus (womb) to prevent pregnancy from developing, thickening the mucus at the cervix (entrance to the uterus) to prevent sperm from entering, and preventing sperm from moving and surviving in the uterus. Levonorgestrel may also prevent ovulation (release of an egg from the ovaries) in some women. Levonorgestrel intrauterine system is an effective method of birth control but it does not prevent the spread of AIDS and other sexually transmitted diseases.
How should this medicine be used?
Levonorgestrel intrauterine system is a small, flexible, T-shaped plastic device to be inserted into the uterus by a health-care provider. The Mirena brand intrauterine systems may be left in place for up to 7 years after it is inserted, the Liletta brand intrauterine systems may be left in place for up to 6 years after it is inserted, the Kyleena brand intrauterine systems may be left in place for up to 5 years after it is inserted, and the Skyla brand intrauterine system may be left in place for up to 3 years after it is inserted. If you still want to use an intrauterine system to prevent pregnancy after this time has passed, your healthcare provider can insert a new system as soon as the old system is removed. The intrauterine systems may be removed by a doctor any time that you want to become pregnant or want to use a different form of birth control. If the Mirena brand intrauterine system is used to treat heavy menstrual bleeding, it may be left in place for up to 5 years after it is inserted.
Your doctor will tell you the best time to have the levonorgestrel intrauterine system inserted. Depending on the timing, you may need to use a non-hormonal birth control method such as condoms and spermicide for 7 days to prevent pregnancy if sexual intercourse occurs. Your intrauterine system may be inserted immediately after a first-trimester miscarriage or abortion. If you have given birth, had a miscarriage, or had a second-trimester abortion, your intrauterine system should not be inserted until at least 6 weeks have passed and a physical exam shows that your uterus has recovered from the pregnancy.
You will need to have your intrauterine system inserted in your health-care provider’s office or clinic. Your health-care provider may tell you to take a nonprescription pain reliever prior to your appointment to help decrease cramping during and after the placement. You may experience some of these symptoms during and after the placement: sweating, pale skin, fast heartbeat, fainting, dizziness, cramping, and bleeding. Tell your health-care provider if your cramping is severe or if these symptoms last for longer than 30 minutes. Your health-care provider will check you to be sure that your system has been placed correctly.
Call your doctor if you experience severe pain during the first few hours after your intrauterine system is inserted. This may be a sign of a serious infection.
Your health-care provider will place your intrauterine system into your uterus, but will leave two threads dangling through your cervix. You should check for these threads once a month so that you will know whether your intrauterine system is still in place. To check for the threads, you should wash your hands with soap and water. Then, reach up to the top of your vagina with clean fingers to feel the threads. If you cannot feel the threads or if you feel any part of the intrauterine system other than the threads, your intrauterine system may not be in place and may not prevent pregnancy. If this happens, call your doctor and use a non-hormonal birth control method such as condoms and spermicide to prevent pregnancy until you are seen by your doctor.
You will need a follow-up appointment with your health-care provider 4-6 weeks after your intrauterine system is inserted to be sure that your system is properly in place. After this appointment, you will need to be examined once every year or more often if you have any problems or concerns.
If your levonorgestrel intrauterine system must be removed, talk to your doctor about the best time to remove it. You are not protected from pregnancy once your intrauterine system is removed, so if you do not want to become pregnant, you will need to be sure that you have effective birth control as soon as your intrauterine system is removed. If you plan to have your intrauterine system replaced with a new intrauterine system, you can have the old system removed and the new system inserted at any time during your menstrual cycle. If you have chosen to use a different form of birth control instead of your intrauterine system and you have regular menstrual cycles, you should have the system removed during the first 7 days after your menstrual period begins and begin using your new form of birth control right away. If you have chosen to use a different form of birth control and you do not have regular cycles, you do not menstruate at all, or you are not able to have your intrauterine system removed during the first 7 days of your menstrual period, you should start using your new form of birth control 7 days before your intrauterine system is removed.
Ask your pharmacist or doctor for a copy of the manufacturer’s information for the patient.
Other uses for this medicine
This medication may be prescribed for other uses; ask your doctor or pharmacist for more information.
What special precautions should I follow?
Before having levonorgestrel intrauterine system inserted,
- Tell your doctor and pharmacist if you are allergic to levonorgestrel, any other medications, or any of the materials used to make levonorgestrel intrauterine system. Ask your pharmacist for a list of the ingredients.
- Tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention the following: anticoagulants (‘blood thinners’) such as warfarin (Jantoven).
- Tell your doctor if you have or have ever had breast cancer or if you think you might have breast cancer and if you have any of the following conditions: any condition that affects the shape of the inside of your uterus including fibroids (growths in or on the uterus that may cause heavy menstrual bleeding, pain, and other symptoms); cancer of the uterus or cervix; unexplained abnormal vaginal bleeding; an untreated infection of the vagina or cervix; pelvic inflammatory disease (PID; an infection of the reproductive organs); any condition that affects your immune system such as leukemia (cancer that begins in the white blood cells) or AIDS (acquired immunodeficiency syndrome); or liver disease or a tumor of the liver. Also tell your doctor if you had a serious infection after pregnancy or abortion in the past 3 months, if you have had PID in the past and have not had a normal pregnancy since your PID got better, if you inject street drugs, if you have more than one sexual partner, or if your partner has more than one sexual partner. Your doctor may tell you not to use a levonorgestrel intrauterine system.
- Tell your doctor if you have ever had a stroke, a heart attack, an ectopic pregnancy (a pregnancy that develops outside the uterus), surgery to treat a problem with your fallopian tubes (tubes that transport eggs that have been released by the ovaries to the uterus), or an abnormal Pap smear (test to detect cancer of the cervix). Also tell your doctor if you have or have ever had a slow heartbeat, heart disease, heart valve disease, high blood pressure, any condition that caused you to faint, severe headaches or migraines, a blood clotting problem, or seizures.
- Tell your doctor if you already have an intrauterine system in place.
- You should not have a levonorgestrel intrauterine system put in place if you are pregnant or plan to become pregnant. Your doctor will give you a pregnancy test before placing your intrauterine system if there is a chance that you might be pregnant.
- You should know about the risks of becoming pregnant while you have an intrauterine system. It is unlikely that you will become pregnant while your intrauterine system is in place, but if you do become pregnant, there is a risk that your pregnancy will be ectopic. Ectopic pregnancies may be life-threatening and may cause internal bleeding or loss of fertility. If your pregnancy is not ectopic, there is a risk that you will develop a severe infection, miscarry, begin labor prematurely, or die if your pregnancy continues with your intrauterine system in place. If you become pregnant with a levonorgestrel intrauterine system in place, you and your doctor should discuss the risks of removing the system. If you continue your pregnancy with the intrauterine system in place, it will increase the risk of miscarriage or infection. You will need to see your doctor often and call immediately if you develop signs of pregnancy loss or infection including flu-like symptoms, fever, chills, cramping, pain, bleeding, or vaginal discharge or leaking. Call your doctor right away if you think you may become pregnant or if you experience symptoms of ectopic pregnancy such as unusual vaginal bleeding or pain in your stomach area at any time while your intrauterine system is in place.
- Tell your doctor if you are breast-feeding. You will probably be able to use levonorgestrel intrauterine system while you are breast-feeding if it is more than 6 weeks after you gave birth.
- You should expect changes in your menstrual cycle while your intrauterine system is in place. Your periods may be irregular, last longer, and be heavier than usual during the first 3-6 months after your intrauterine system is put in place. You may experience spotting or light bleeding between periods during this time. As time passes, your periods may become lighter and shorter or may stop completely. If your period stops, it will return when your intrauterine system is removed. Call your doctor if you have been having periods but have not had one in 6 weeks, or if your bleeding had become light for a time but becomes heavy.
- You and your partner will not be able to feel your intrauterine system during intercourse because the system will be placed inside your uterus. However, your partner may feel the threads. Call your doctor if this happens.
- You should know that there is a risk that your intrauterine system will become attached to the wall of your uterus or may move through the wall of your uterus, causing damage or scarring to other organs. If this happens, you might need surgery to remove the system. There is a higher risk that your intrauterine system will move through the wall of your uterus if you are breast-feeding.
- You should know that using a levonorgestrel intrauterine system may increase the risk that you will develop PID. PID may cause infertility, ectopic pregnancy, pain that does not go away, and death. Sometimes PID must be treated with surgery, including hysterectomy (surgery to remove the uterus). The risk that you will develop PID is higher if you or your partner have more than one partner. Call your doctor if you experience any of the following symptoms of PID: long-lasting or heavy bleeding, unusual vaginal discharge, stomach area pain, painful sex, chills, or fever.
What special dietary instructions should I follow?
Unless your doctor tells you otherwise, continue your normal diet.
What side effects can this medication cause?
Levonorgestrel intrauterine system may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- Headache
- Acne
- Breast tenderness
- Nausea
- Weight gain
- Cramps or pain during menstruation
- Decreased sexual desire
- Depression
- Changes in mood
- Hair loss
- Unwanted hair growth
Some side effects can be serious. If you experience any of these symptoms or those mentioned in the SPECIAL PRECAUTIONS section, call your doctor immediately or get emergency medical treatment:
- Foul-smelling or unusual vaginal discharge
- Vaginal pain
- Pain during sex
- Sores on the genital area
- Yellowing of the skin or eyes
- Sudden weakness of an arm or leg
- Drooping of one side of the face
- Difficulty speaking or understanding
- Crushing chest or shoulder pain
- Swelling of the lips, tongue, throat, arms, hands, legs, or feet
- Rash
- Hives
Levonorgestrel intrauterine system may increase the risk that you will develop a cyst on your ovary. This type of cyst may cause pain but will usually disappear in 2-3 months. In rare cases, surgery to remove the cyst may be needed. Talk to your doctor about the risks of using a levonorgestrel intrauterine system.
Levonorgestrel intrauterine system may cause other side effects. Call your doctor if you have any unusual problems while your intrauterine system is in place.
If you experience a serious side effect, you or your doctor may send a report to the Food and Drug Administration’s (FDA) MedWatch Adverse Event Reporting program online (http://www.fda.gov/Safety/MedWatch) or by phone (1-800-332-1088).
What other information should I know?
Keep all appointments with your doctor.
If you have a Skyla or Kyleena brand intrauterine system, tell your doctor and the radiology staff that you have one of these types of intrauterine system before you undergo a magnetic resonance imaging (MRI) scan.
Ask your pharmacist any questions you have about levonorgestrel intrauterine system.
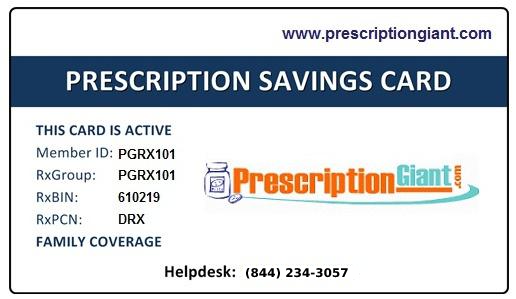
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Brand names
- Kyleena®
- Liletta®
- Mirena®
- Skyla®