WARNING
Gleostine (lomustine) is a chemotherapy medication used to treat certain types of cancer, including brain tumors and Hodgkin’s lymphoma. Like many chemotherapy drugs, Gleostine carries several risks and potential side effects:
- Bone marrow suppression: Gleostine can lower your body’s ability to produce blood cells, leading to anemia (low red blood cells), leukopenia (low white blood cells), and thrombocytopenia (low platelets).
- Increased risk of infection: Due to lowered white blood cell count, individuals taking Gleostine are more susceptible to infections.
- Nausea and vomiting: Common side effects of Gleostine treatment include nausea and vomiting, which can sometimes be severe.
- Liver toxicity: Gleostine can cause liver damage, which may lead to elevated liver enzymes or liver failure.
- Pulmonary toxicity: Rarely, Gleostine may cause lung problems such as pulmonary fibrosis, which can impair breathing.
- Increased risk of secondary cancers: Long-term use of Gleostine may increase the risk of developing secondary cancers.
- Reproductive risks: Gleostine can harm the developing fetus, so it should not be used during pregnancy. It may also affect fertility in both men and women.
It’s crucial for patients taking Gleostine to be closely monitored by their healthcare team for these potential risks and side effects. Additionally, patients should discuss with their doctor the benefits and risks of Gleostine treatment, as well as any concerns or questions they may have.
Why is this medication prescribed?
Gleostine (lomustine) is prescribed primarily for the treatment of certain types of cancer, particularly brain tumors and Hodgkin’s lymphoma. It belongs to a class of chemotherapy drugs called alkylating agents, which work by interfering with the DNA of cancer cells, ultimately preventing their growth and replication.
How should this medicine be used?
Here are general guidelines on how Gleostine is commonly used:
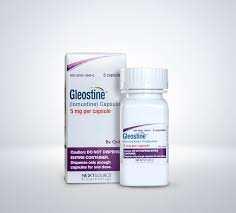
- Administration: Gleostine is typically taken orally in the form of capsules.
- Dosage: The dosage of Gleostine varies depending on factors such as the type of cancer being treated, the patient’s overall health, and other medications they may be taking. Dosage is usually determined by the prescribing healthcare provider.
- Frequency: Gleostine is often given as a single dose every 6 weeks, although the exact dosing schedule may vary based on individual circumstances.
- Monitoring: Patients receiving Gleostine should undergo regular blood tests to monitor their blood cell counts and liver function, as well as to assess for any potential side effects.
- Precautions: It’s essential to follow the instructions provided by the healthcare provider and pharmacist carefully. Gleostine should be taken exactly as prescribed, and patients should not alter the dosage or frequency without consulting their doctor.
- Handling: Gleostine capsules should be handled with care, and precautions should be taken to avoid direct contact with the skin or inhalation of the medication dust. If capsules are broken or damaged, they should not be handled directly, and gloves should be worn when handling them.
- Storage: Gleostine should be stored at room temperature away from moisture and heat. It should be kept out of reach of children and pets.
As with any chemotherapy medication, it’s crucial for patients to communicate closely with their healthcare team throughout treatment to monitor for any potential side effects and adjust the treatment plan as needed.
Other uses for this medicine
While Gleostine (lomustine) is primarily used in the treatment of certain types of cancer, including brain tumors and Hodgkin’s lymphoma, it may also be prescribed for other conditions or off-label uses as determined by healthcare providers. Some off-label uses of Gleostine may include other types of cancer or conditions where its mechanism of action may be beneficial, although such uses would be at the discretion of the prescribing physician.
What special precautions should I follow?
Special precautions to follow when taking Gleostine:
- Pregnancy and breastfeeding: Gleostine can harm the developing fetus, so it should not be used during pregnancy. Women of childbearing age should use effective contraception during treatment and for some time afterward. It’s also recommended to avoid breastfeeding while taking Gleostine, as it may pass into breast milk and harm the nursing infant.
- Liver function: Patients with pre-existing liver disease or impairment should be closely monitored while taking Gleostine, as it can cause liver toxicity. Liver function tests should be performed regularly to assess for any signs of liver damage.
- Blood cell counts: Gleostine can cause bone marrow suppression, leading to low blood cell counts (anemia, leukopenia, thrombocytopenia). Patients should undergo regular blood tests to monitor their blood cell counts, and treatment may need to be adjusted accordingly.
- Infections: Due to decreased white blood cell counts, patients taking Gleostine are more susceptible to infections. It’s essential to practice good hygiene and avoid exposure to sick individuals. Promptly report any signs of infection to your healthcare provider.
- Kidney function: Patients with pre-existing kidney problems should be monitored while taking Gleostine, as it can affect kidney function. Adjustments to the dosage may be necessary in individuals with impaired kidney function.
- Fertility: Gleostine may affect fertility in both men and women. It’s advisable to discuss fertility preservation options with your healthcare provider before starting treatment if fertility preservation is a concern.
- Handling precautions: Gleostine capsules should be handled with care, and precautions should be taken to avoid direct contact with the skin or inhalation of the medication dust. If capsules are broken or damaged, they should not be handled directly, and gloves should be worn when handling them.
- Interactions: Inform your healthcare provider about all medications, supplements, and herbal products you are taking, as they may interact with Gleostine and affect its effectiveness or increase the risk of side effects.
As always, it’s crucial to follow the instructions provided by your healthcare provider and pharmacist closely and to communicate any concerns or questions you may have about Gleostine treatment.
What special dietary instructions should I follow?
There are no specific dietary restrictions associated with Gleostine. However, maintaining a healthy and balanced diet can support overall health and may help manage potential side effects such as nausea and vomiting. Some individuals may find it helpful to eat smaller, more frequent meals and to avoid spicy, greasy, or heavy foods if they experience gastrointestinal side effects.
What should I do if I forget a dose?
What side effects can this medication cause?
Gleostine (lomustine), like many chemotherapy medications, can cause a range of side effects, which can vary in severity from person to person. Some common side effects of Gleostine include:
- Nausea and vomiting: These are among the most common side effects of chemotherapy drugs, including Gleostine. Anti-nausea medications may be prescribed to help manage these symptoms.
- Bone marrow suppression: Gleostine can lower the production of blood cells in the bone marrow, leading to anemia (low red blood cells), leukopenia (low white blood cells), and thrombocytopenia (low platelets). This can increase the risk of infection, bleeding, and fatigue.
- Liver toxicity: Gleostine can cause liver damage, which may manifest as elevated liver enzymes in blood tests. Symptoms of liver toxicity may include jaundice (yellowing of the skin and eyes), abdominal pain, and dark urine.
- Pulmonary toxicity: Although rare, Gleostine may cause lung problems such as pulmonary fibrosis, which can lead to shortness of breath, coughing, and difficulty breathing.
- Nervous system effects: Some individuals may experience neurological side effects such as confusion, dizziness, or weakness.
- Gastrointestinal symptoms: In addition to nausea and vomiting, Gleostine may cause other gastrointestinal side effects such as diarrhea, constipation, or loss of appetite.
- Hair loss: Chemotherapy drugs like Gleostine can lead to hair thinning or hair loss, although this is usually temporary and hair typically regrows after treatment is completed.
- Fertility effects: Gleostine may affect fertility in both men and women. It’s important to discuss fertility preservation options with your healthcare provider before starting treatment if fertility preservation is a concern.
- Increased risk of secondary cancers: Long-term use of Gleostine may increase the risk of developing secondary cancers.
It’s essential to communicate any side effects or concerns you experience with your healthcare provider, as they can provide guidance and support to help manage side effects and improve your overall treatment experience. Additionally, some side effects may require prompt medical attention, so it’s crucial to seek medical help if you experience severe or concerning symptoms.
What should I know about storage and disposal of this medication?
Storage and disposal of Gleostine:
- Storage: Gleostine capsules should be stored at room temperature away from moisture and heat. Keep them in their original packaging and out of reach of children and pets.
- Disposal: Unused or expired Gleostine capsules should be disposed of properly according to local regulations. Do not flush them down the toilet or pour them down the drain unless instructed to do so. Consult your pharmacist or healthcare provider for guidance on the proper disposal of unused medications.
In case of emergency/overdose
In case of emergency/overdose of Gleostine:
- Seek medical attention: If you suspect an overdose of Gleostine or experience severe side effects such as difficulty breathing, loss of consciousness, or severe nausea and vomiting, seek emergency medical assistance immediately.
- Poison Control: You can also contact your local poison control center or emergency department for guidance on managing an overdose of Gleostine.
What other information should I know?
- Follow-up appointments: Attend all scheduled follow-up appointments with your healthcare provider while taking Gleostine. These appointments are essential for monitoring your response to treatment, managing side effects, and adjusting your treatment plan as needed.
- Medication interactions: Inform your healthcare provider about all medications, supplements, and herbal products you are taking, as they may interact with Gleostine and affect its effectiveness or increase the risk of side effects.
- Dietary considerations: While there are no specific dietary restrictions associated with Gleostine, maintaining a healthy and balanced diet can support overall health and may help manage potential side effects such as nausea and vomiting.
- Supportive care: Seek support from family, friends, or support groups to cope with the emotional and physical challenges of cancer treatment. Your healthcare provider can also provide resources and referrals to support services as needed.
- Follow instructions carefully: Always follow the instructions provided by your healthcare provider and pharmacist closely when taking Gleostine. Do not alter the dosage or frequency of administration without consulting your doctor.
- Pregnancy and breastfeeding: As mentioned earlier, Gleostine can harm the developing fetus, so it should not be used during pregnancy. Effective contraception should be used during treatment and for some time afterward. Gleostine should also be avoided while breastfeeding.
- Driving and operating machinery: Gleostine may cause dizziness or weakness, which can impair your ability to drive or operate machinery. Avoid these activities if you experience such side effects while taking Gleostine.
Always consult your healthcare provider or pharmacist if you have any questions or concerns about Gleostine or its use.